Caesarean Section Pros and Cons: What to Know
Welcoming a new life is a big step, and choosing how to deliver is key. Caesarean section, or c-section, is a common choice in the U.S., making up nearly one-third of births. It’s a lifesaver in some cases but also comes with its own set of risks and considerations. This guide will help you understand the pros and cons of c-sections, so you can make a choice that fits your needs and preferences.
Table of Contents
Understanding Cesarean Section
Definition and Overview
A cesarean section, or C-section, is a surgery where a baby is born through cuts in the mother’s belly and uterus. The surgeon goes through layers of skin, fat, muscles, and the uterus to get to the baby.
Anatomy and Physiology Involved
The uterus is key in a C-section. It has three layers: the outer perimetrium, the middle myometrium, and the inner endometrium. Each layer must be cut to reach the baby.
The cuts in a C-section let the surgeon bring the baby out safely. This method is chosen for many reasons, like past C-sections, certain placenta issues, or if the baby is in distress.
Indications for Cesarean Section
Cesarean deliveries are common in the United States, with over a million each year. They are divided into three main reasons: maternal, uterine/anatomic, and fetal indications.
Maternal Indications
Some reasons for a cesarean include a previous cesarean, a mother’s request, or certain medical conditions. These can make vaginal delivery risky for the mother.
Uterine/Anatomic Indications
Uterine or anatomic issues might require a cesarean. These include abnormal placentation or invasive cervical cancer. These conditions can block the birth canal or threaten the health of mother and baby.
Fetal Indications
Fetal reasons for a cesarean include nonreassuring fetal status or umbilical cord prolapse. Other reasons are malpresentation, macrosomia, and congenital anomalies. These make vaginal delivery unsafe or impossible.
About 1 in 3 births in the United States are cesarean sections. This includes 16 in 100 planned and 17 in 100 emergency cesareans. The procedure involves a 10 to 15 cm cut at the abdomen’s bottom. It takes about 10 minutes to deliver the baby and 30 to 40 minutes to close the stitches.
While the cesarean rate might not drop soon, knowing the reasons helps parents decide. This knowledge is key for informed choices about delivery options.
Caesarean Section Pros and Cons
Caesarean deliveries, or C-sections, offer benefits for both mothers and babies. Yet, they also come with risks and complications. Knowing the pros and cons helps you decide on your delivery method.
Benefits of Cesarean Delivery
- Prevents complications: Caesarean sections can avoid issues like placenta or umbilical cord problems, or labor distress.
- Allows for a planned delivery: You can plan the birth timing and logistics, which is helpful in some cases.
- Reduces pelvic floor damage: They can prevent pelvic floor injuries that might happen in vaginal births.
Risks and Complications
Caesarean sections have benefits but also risks and complications. These include:
- Increased risk of infection: There’s a higher chance of infections like in the uterus, bladder, or incision site.
- Bleeding and blood clots: There’s a higher risk of bleeding too much or getting blood clots during and after the surgery.
- Longer recovery time: Recovery from a C-section takes longer, often three months or more.
- Future pregnancy complications: They might raise the risk of problems in future pregnancies, like placental issues or uterine rupture.
Choosing a C-section should be a decision made with your healthcare provider. They can help you understand the benefits and risks based on your situation.
“Caesarean sections can be a lifesaving procedure, but it’s important to understand the potential risks and challenges involved. Open communication with your healthcare team is key to making an informed decision about your delivery method.”
Preparing for a Cesarean Birth
Getting ready for your cesarean section involves several steps for a smooth experience. Preparing for a c-section, what to expect before a cesarean, and cesarean section preparation are key. They help you prepare well.
Start by attending all pre-operative appointments with your healthcare provider. These meetings let you discuss the procedure and ask questions. You’ll also get detailed instructions on how to prepare. Your provider will likely tell you to arrange for childcare and transportation to and from the hospital.
Follow any dietary or medication instructions from your healthcare team. This might mean fasting before the procedure or adjusting your medication schedule. Following these guidelines makes the surgery safer and more efficient.
In the days before your cesarean section, pack a hospital bag with essentials. Include comfortable clothing, toiletries, and items that make you feel at ease. Also, talk to your provider about your birth experience preferences, like skin-to-skin contact or delayed cord clamping.
Remember, preparing for a cesarean birth is a team effort. By being proactive and following your healthcare team’s advice, you’ll feel confident and empowered. This is a big milestone.
The Surgical Procedure
A cesarean section, or C-section, is a surgery to deliver a baby through the mother’s abdomen and uterus. It’s chosen when vaginal delivery is risky for the mother or baby.
Step-by-Step Process
The cesarean section procedure involves these steps:
- Anesthesia is given, like spinal, epidural, or general, based on the situation.
- The surgeon makes a cut in the lower abdomen, usually a horizontal one just above the pubic bone.
- Then, the surgeon opens the uterus and takes out the baby.
- The placenta is removed, and the uterus is stitched up.
- The cut in the abdomen is closed with stitches or staples.
The whole procedure usually takes 10 to 15 minutes.
Anesthesia Options
The choice of anesthesia for a cesarean depends on several factors. These include the urgency of the delivery, the mother’s health, and the healthcare team’s preference. The most common options are:
- Spinal anesthesia: A single injection into the spinal cord, numbing the abdomen and below.
- Epidural anesthesia: A catheter in the epidural space for continuous pain relief.
- General anesthesia: The mother is put to sleep, with a breathing tube for oxygen.
About 5% to 10% of cesarean sections use general anesthesia. Most use spinal or epidural anesthesia.
Recovery After Cesarean Section
Recovering from a cesarean section, or C-section, is a big deal. It takes patience and care. Your healthcare team will watch you closely for any problems. They will also guide you on how to care for yourself and manage pain.
Postoperative Care
After a C-section, you’ll likely stay in the hospital for 3-5 days. Some places might let you go home in 2-3 days. Your healthcare team will check on your incision, bleeding, and overall health.
You might bleed a lot at first, like during a heavy period. You’ll need to use maternity pads for up to 6 weeks. It takes 6-10 weeks for the incision to fully heal.
Your healthcare team will tell you when you can start doing things like driving and lifting again. They’ll also say when you can do more strenuous activities. Walking a bit is okay a few days after surgery.
Pain Management
Managing pain after a C-section is key. Your healthcare team will help you find a pain plan. This might include medicines and non-medical methods like ice packs and massage.
Make sure to follow your pain medicine plan. This helps you heal and feel better. You’ll have a 6-week checkup to make sure you’re recovering well.
| Postoperative Milestone | Average Timeline |
|---|---|
| Hospital Stay | 3-5 days (some hospitals allow 2-3 days) |
| Incision Healing | 6-10 weeks |
| Resuming Driving | 4-6 weeks |
| Postpartum Checkup | 6 weeks |
Gentle Cesarean: A Family-Centered Approach
Cesarean sections are now common, with about one in three births in the U.S. being C-sections. A new method, known as “gentle” or “natural” cesarean, has emerged. It aims to make the delivery more engaging and bonding, while keeping it safe.
The gentle cesarean technique includes playing soothing music and dimming the lights. It also allows for immediate skin-to-skin contact between the newborn and parents. The doctor makes a smaller incision, like a “natural” or “bikini-line” incision, to reduce scarring.
One big plus of a gentle cesarean is the chance for more parental involvement and bonding. Seeing the baby’s birth and having skin-to-skin contact right away makes the experience more intimate. This is especially good for those who wanted a vaginal birth but needed a cesarean.
Gentle cesareans also have similar safety and recovery outcomes as traditional C-sections. They have the same rates of infection, bleeding, and other complications. But, they offer a more family-centered experience.
If you’re thinking about a cesarean, talk to your healthcare provider about a gentle or natural approach. Knowing the benefits can make your birthing experience more positive, even with a surgical delivery.
“The gentle cesarean allows for a more intimate and memorable birth experience, while still prioritizing the safety and well-being of the mother and child.”
| Gentle Cesarean | Traditional Cesarean |
|---|---|
| Smaller incision, often “bikini-line” | Larger incision on the abdomen |
| Immediate skin-to-skin contact with newborn | Newborn separated from parents initially |
| Dimmed lights and soothing music | Bright, clinical environment |
| Increased parental involvement and bonding | More clinical, less personal experience |
Choosing a gentle cesarean means a more family-centered birthing experience. It balances the medical needs of a C-section with the emotional needs of the family. This approach is a thoughtful mix of clinical safety and family bonding.
Vaginal Birth After Cesarean (VBAC)
Some people who had a cesarean before might choose a vaginal birth after cesarean (VBAC). Whether you can have a VBAC depends on several things. These include the type of cut made in your uterus, why you had a cesarean before, and the risks and benefits for you and your baby.
Eligibility and Considerations for VBAC
Research shows that up to 75% of people who had one C-section can have a successful vaginal birth later. But, if you’ve had two or more C-sections, the success rate drops to about 50%.
The kind of cut made during your C-section matters a lot. A low transverse incision is safer for VBACs. But, a high vertical incision, or “classical” incision, is riskier. People with multiple C-sections face higher risks like heavy bleeding and uterine rupture.
Other things can also affect your chances of a successful VBAC:
- Previous C-section deliveries with low transverse incisions
- History of vaginal birth
- Absence of uterine surgeries
- No history of uterine rupture
- Absence of certain medical conditions
- Labor starting naturally before the due date
Women with preeclampsia might face a C-section over a vbac. Age, obesity, and a big baby can also make a VBAC less likely. So can being overdue, having twins, or having a short time between pregnancies.
But, if you’ve had a successful VBAC before, you’re more likely to have one again. It’s key to talk to your healthcare provider about your situation. They can help decide what’s best for you and your baby.
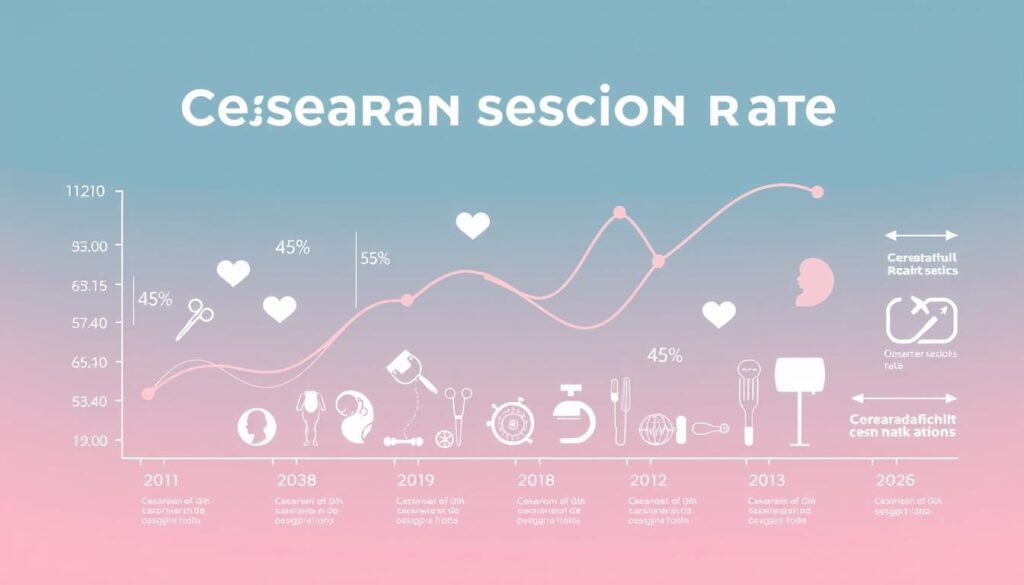
Cesarean Rates and Trends
The cesarean delivery rate in the United States has gone up a lot. It was 5% in 1970 and 31.9% in 2016. This rise is due to many reasons, like older moms, new medical tools, and changes in how doctors help with births. Now, there are efforts to lower the cesarean rate. This includes helping moms have vaginal births after a cesarean and supporting natural labor when it’s safe.
The World Health Organization (WHO) says the best cesarean rate is 10-15%. But, many places have seen more cesarean deliveries than this.
| Region | Cesarean Section Rate |
|---|---|
| Latin America and the Caribbean | 40.5% |
| North America | 32.3% |
| Europe | 25.0% |
| Asia | 19.2% |
| Africa | 7.3% |
Many things contribute to the rise in cesarean section rates and trends in c-section deliveries. These factors differ by region and country. It’s important to understand these trends and reasons. This helps in creating plans to improve maternity care that is based on evidence and focuses on the patient.
“Every effort should be made to make caesarean sections available to women in need rather than aiming for a specific quota.”
– World Health Organization
Communicating with Your Healthcare Team
Talking openly with your healthcare team is key when deciding how to deliver your baby. Share your likes, concerns, and any questions about a cesarean section or other options. They can explain the risks and benefits, helping you choose what’s best for you.
It’s important to be clear with your doctor about your cesarean thoughts. Share your thoughts, likes, and any fears. Your doctor can talk about the medical side and help you understand the options for a cesarean section. This way, you can plan a delivery that fits your needs and keeps you and your baby safe.
Your healthcare team is here to support you. Don’t be shy about asking questions or sharing your worries. Good communication with your provider makes you feel strong and sure about your delivery choices.